With more than 2,000 on the road in the U.S. and performing 6-½ million visits annually mobile health clinics serve an important role in the health care system, providing care to some of the most vulnerable populations. Between 2007 and 2017 Mobile Health Map monitored 811 participating clinics to identify:
- The demographics they serve
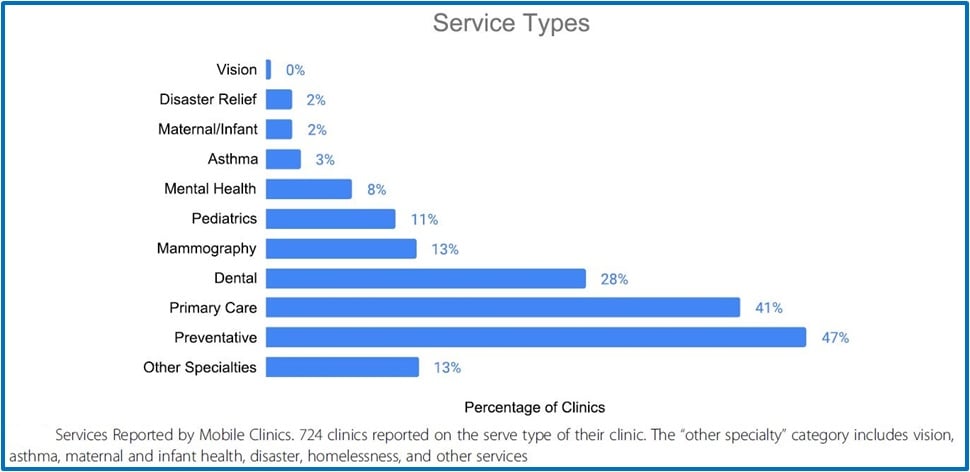
- The services they provide
- Their affiliated institutions and funding sources
Included in their findings it was identified that:
- Mobile clinics provide a median number of 3,491 visits annually
- More than half of the clients are women at 55%
- 59% are of racial/ethnic minorities
- 146 clinics reported insurance data identifying:
- 41% of clients were uninsured
- 44% had some form of public insurance
- 41% of the service models were primary care
- 47% focused on prevention
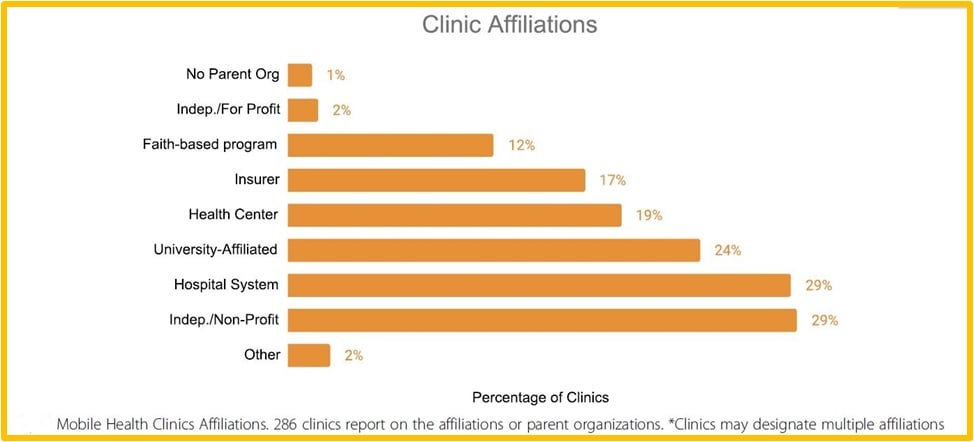
Their organizational affiliations varied from:
- 33% being independent
- 24% were affiliated with a university
- 29% are part of a hospital or health care system
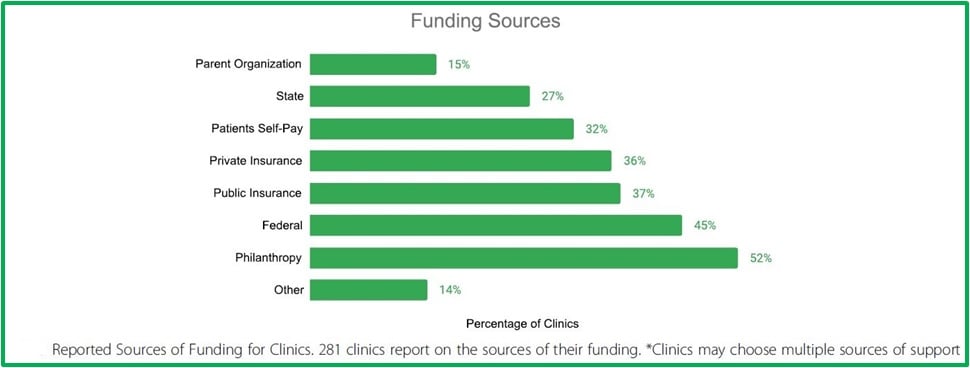
Primary sources of financial support come from:
- 52% philanthropy
- 45% federal funds
For nearly half a century mobile health care has been innovating the health services delivery landscape by providing a wide variety of services to vulnerable populations. Mobile clinics vary in the types of services they provide, patient demographics they target, and relationships with a fixed health system. Although the Affordable Care Act has helped with access to care in recent years, some barriers continue to persist, particularly among {{cta(’65f281b8-a8e6-46c6-a1fa-084f2b437246′,’justifyright’)}}populations living in areas with limited resources, such as Native American Reservations, parts of Appalachia, and other impoverished rural and urban areas. Beyond serving individuals on-site, mobile health clinics enhance access between the community and clinical facilities.
Affiliations
Major healthcare institutions such as hospitals and universities can make the biggest impact on the broader community due to their resources and reach. Of 286 clinics surveyed 29% were affiliated with hospital systems and 24% were with universities. This shows a strong representation, however many hospital chains and larger universities do not take advantage of this tremendous opportunity which can lead patients back to the home institution for further treatments, providing a broader revenue stream. Most of the balance of providers was independent for profit or non-profit programs representing 31% of the total.
In addition, 19% of respondents are affiliated with community health centers, 17% with insurance companies, and 12% with faith-based organizations.
It’s important to note that many clinics may designate multiple affiliations, such as Kaiser Permanente which is a health system and insurer.
Funding Sources
As reported by Mobile Health Map mobile health clinics save the U.S. healthcare system $12 for every $1 invested in the mobile health sector. This illustrates the significant return-on-investment for institutions that provide mobile health services to their communities. Of those surveyed:
- 173 mobile clinics reported an average annual operating cost of $632,369.
- 58 clinics designated themselves as a prevention clinic (i.e. mammography screenings, which excludes primary care), averaging $319,868 in annual operating cost.
- Another 58 primary care clinics reported an average of $981,092 per year.
- 37 dental clinics reported an average of $1,169,559 on annual operations.
Though there is an ROI to be realized with a mobile health clinic program, most still need to depend on government funding and philanthropy. Of the clinics surveyed 281 reported where their sources of funding com from:
- 45% reported federal funding
- 52% reported support through philanthropic organizations or private individuals
- 37% received support from public insurance providers
- 36% from private insurance
- 32% of clinics reported receiving revenue from patient self-pay
- Additional sources of revenue were reported such as parent organizations at 15% and state funding at 27%
As with their affiliations, many clinics may designate multiple funding sources.
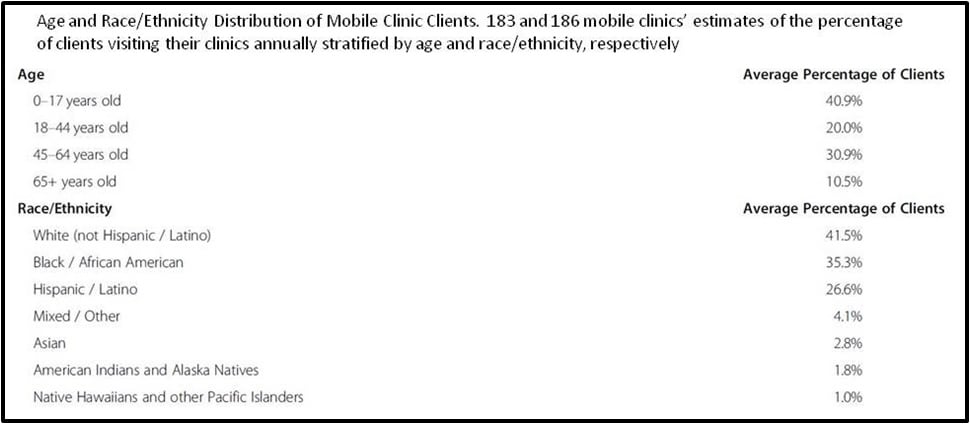
Client Demographics
Of the 811 mobile clinics participating in the study, 253 reported information on the total number of annual visits establishing a median number of 3,491 visits per year. In addition, new visits were reported by 166 clinics averaging 2,713 annually.
Gender distribution was reported by 192 participants with female clients representing a slight majority of 55%, with 44% being male.
In addition, 166 clinics reported data on the percentages of race/ethnicity of clients who visited their clinics. The highest percentage was white at 42%, Black/African-American at 35%, and Hispanic clients at 27%. The combined percentage of Asians, Native American, multiracial, and those clients designating their ethnicity as “other” were less than 10%.
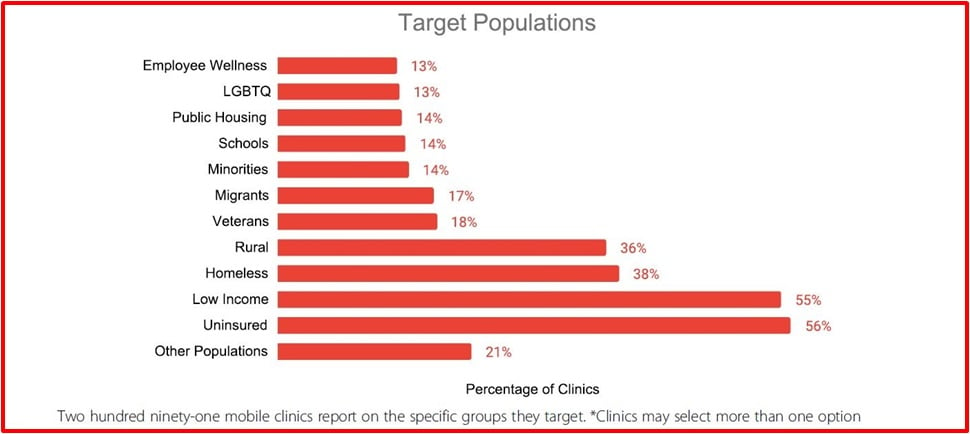
The goal of most mobile clinics is to reach populations with limited access to care. To understand which client populations clinics serve they were asked to report the group or groups they target. The 291 clinics reporting the target populations they service ranges from the uninsured, low-income groups, homeless persons, to rural communities. Many target multiple populations and institutions that may include schools, public housing, veterans, LGBTQ individuals and more.
Of the 811 participating clinics, most of them (724) reported on the service type(s) their clinics provide.
Targeted populations and services provided are illustrated below
Why Mobile Health Clinics
Mobile health clinics deliver care to some of the country’s most vulnerable populations, including people of color, those experiencing poverty and/or homelessness and the uninsured. Care is provided to rural and urban communities, veterans, immigrants and Native American communities. These clinics not only operate across America, but around the world and are supported with the financial support of health care systems, universities, philanthropy, and government agencies.
The people and organizations that operate mobile clinics are often motivated by a commitment to underserved communities and use mobile health clinics as a vehicle to deliver care in ways that differ from traditional medical settings. For example, a mobile clinic in Boston commented their goal is to create a culture of respect and inclusivity for their clients. Mobile clinics frequently serve as a bridge between these disenfranchised communities and the health care system. As health care leaders and policymakers increasingly recognize the importance of social determinants of health and community-clinical linkages, mobile clinics are well-positioned to bridge the gap.
Mobile Units Used for Services Beyond Traditional Healthcare
Traditional mobile healthcare services are in the areas of dental, women’s health, blood mobiles, and family medicine. However, there are many other applications for mobile clinics that go beyond the traditional, such as programs that provide regulatory compliance screenings for industry:
- The National Institute for Occupational Safety and Health (NIOSH) for the Coal Workers’ Health Surveillance Program’s (CWHSP) screenings for black lung disease.
- Summa Health System Occupational/Corporate Health an Ohio Bureau of Worker’s Compensation (BWC) provider offering comprehensive occupational health services.
- Bio-Care, an independent organization helping companies meet regulatory compliance requirements while enhancing employee health and safety.
Conclusion
While mobile clinics exist across the country, many underserved rural areas and under-resourced urban areas continue to suffer from health disparities that could be addressed by expanding the network of mobile clinics. With an increasing emphasis on population health and meeting people where they work, live, and play, understanding why and how these systems operate can inform effective community-clinical linkages.
Mobile clinics reduce barriers to health care and address the social determinants of health by providing access, saving time, reducing complexity in the system, and developing trust. They are an integral part of the health care system and are financially supported by government agencies, insurance companies, and philanthropy. To advance health equity and reach the most vulnerable and disenfranchised populations, we need to increase investment in mobile clinics and other innovative ideas that promote preventive services and expand the boundaries of the traditional health care system.
This article was prepared using material directly, in part and with some editing without contradiction to original source material under the terms of the Creative Commons Attribution 4.0, International License (https://creativecommons.org/licenses/by/4.0. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in the original article, unless otherwise stated.
Original source material authors: Nelson C. Malone, Mollie M. Williams, Mary C. Smith Fawzi, Jennifer Bennet, Caterina Hill, Jeffrey N. Katz and Nancy E. Oriol