In 2017, drug overdose deaths in the United States were more than 70,000, which is almost 200 per day. This was nearly a 10 percent increase from 2016.
From 1999 to 2017, over 702,000 Americans have died from drug overdoses, and over 10 percent of those were in 2017. In addition, an in-depth CDC analysis report indicated overdose death rates linked to synthetic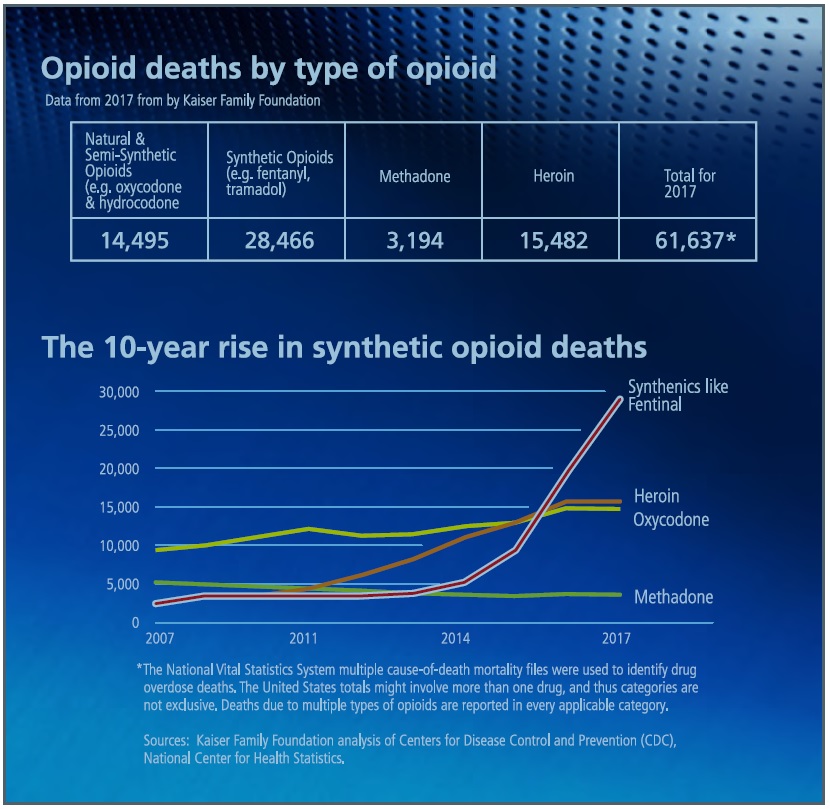 opioids, including illicitly manufactured fentanyl, experienced a dramatic 150 percent increase in 2017.
opioids, including illicitly manufactured fentanyl, experienced a dramatic 150 percent increase in 2017.
For two specific demographics during the 2016 to 2017 period the highest percent increase in opioid-involved deaths were among blacks at 25.2 percent and adults over age 65 at 17.2 percent (an alarming statistic).
What is Being Done?
The U.S. Department of Health and Human Services (HHS) is leading programs at the national level to respond to and help prevent drug overdoses of all types, primarily those involving opioids. The HHS has implemented a five-point strategy to combat opioid addiction:
Access:
- Access: Better Prevention, Treatment and Recovery Services
-
In September 2018, HHS awarded over $1 Billion to combat the opioid crisis
-
-
Data: Better Data on the Epidemic
-
HHS is improving their understanding of the crisis by supporting timely and specific public health data and reporting, including the acceleration of CDC’s reporting of drug overdose data
-
-
Pain: Better Pain Management
- Identifying alternative pain-management practices and prescribing guidelines.
- Identifying alternative pain-management practices and prescribing guidelines.
-
Overdoses: Better Targeting of Overdose-Reversing
-
HHS is working to make lifesaving overdose-reversing drugs more readily available
-
-
Research: Better Research on Pain and Addiction
-
HHS is supporting cutting-edge research on pain and addiction.
-
On a state, regional and local level, behavioral health programs, rehabilitation clinics and hospitals are expanding their reach with an increase in programs such as mobile healthcare vehicles to help those suffering from addictions.
Mobile Health Units on the Front Lines
One of the biggest assets to tackling this crisis is mobile healthcare vehicles. Deployed to rural communities, urban neighborhoods, schools, prisons and retail centers, these mobile units are a visible sign to those who find it difficult to accept help on their own. They serve to overcome the stigma of seeking initial help at hospitals, doctor’s offices or even drug-treatment facilities. Mobile health units can reach those in the  shadows, struggling with addictions and too fearful or paranoid to seek help. It is also widely known that this epidemic is not just “on the street”; it is also prevalent in middle and upper class America, schools, businesses and every walk of life.
shadows, struggling with addictions and too fearful or paranoid to seek help. It is also widely known that this epidemic is not just “on the street”; it is also prevalent in middle and upper class America, schools, businesses and every walk of life.
The primary functions of most mobile healthcare programs, focusing on the opioid crisis are the following:
- Addiction Services: Screenings, medications for addiction treatment, referrals to opioid and other drug addiction-treatment programs, in-patient detoxification and counseling services.
- Harm Reduction: Overdose-prevention education, administering Naloxone, risk-reduction counseling and syringe exchange.
- Preventive Care:Chronic disease management (including hypertension, diabetes, HIV treatment), hepatitis C treatment, immunizations, referrals to behavioral-health specialists, health and drug screenings and other services based on patient needs.
Health Resources and Services Administration: Opioid Response Planning Grants
To battle this epidemic where people are cutoff or have cut themselves off from society, many community health centers, universities, hospitals and other local organizations are going to the field with mobile health clinics. The Health Resources and Services Administration (HRSA) and the Office of Rural Health (ORH) has awarded Rural Communities Opioid Response Planning grants (RCORP-Implementation funds) to be used to form a consortium of local health care organizations, substance use treatment providers and other human  service agencies. Among other services, these grants are helping to acquire mobile health clinics built specifically for addiction treatment and behavioral health.
service agencies. Among other services, these grants are helping to acquire mobile health clinics built specifically for addiction treatment and behavioral health.
One example is CareSouth Carolina of Hartsville, South Carolina working in conjunction with Rubicon, ALPHA Behavioral Health Center and Trinity Behavioral Care. With the help of an HRSA grant they put their new Freedom ROADS mobile healthcare unit in service in February 2019 to provide Medication Assistance Treatment services (MAT) on-site at several locations on a pre-scheduled route in their region. According to CareSouth Carolina, this MAT mobile unit provides FDA-approved medications, in combination with counseling and behavioral health, to give a “whole-patient” approach to the treatment of substance-use disorders.
HRSA grants are provided to organizations to support the improvement and expansion of health care services for underserved populations. “Nationwide, nearly 1,400 health-center grantees operate approximately 12,000 fixed sites and mobile medical units, providing affordable primary and preventive care on a sliding fee scale to more than 27 million patients.” The HRSA provides the information on how grants and funding are distributed per state and how those funds are allocated. Consider for instance the state of Texas which experienced a marked increase in overdose deaths caused by synthetic opioids in 2017. The chart below illustrates the impact the HRSA had in working with Texas in 2018:
Total Awards – Texas
|
Program |
FY 2018 Funding |
Distinct Grantees |
Distinct Grants |
|
Grants and Cooperative Agreements |
$574,535,975 |
136 |
252 |
|
Loans and Scholarships |
$5,993,898 |
125 |
N/A |
|
Opioid Crisis Response |
$16,327,642 |
N/A |
N/A |
Federally Qualified Health Centers (FQHCs)
Many Federally Qualified Health Centers (FQHCs) utilize mobile clinics as a primary resource for improving access to health care for substance abuse disorders and other much needed health services in housing projects, rural areas, urban communities and for homeless populations. Incorporating mobile care units into a healthcare system provides opportunities for outreach, raising awareness about the local community’s health center and working to serve the disenfranchised and individuals who are isolating themselves when battling addictions.
FQHCs can play a key role in how mobile health clinics work with schools, employers and other community partners to collaborate with local hospitals and substance abuse centers.
Conclusion
Mobile medical clinics (MMCs) are non-traditional methods for providing healthcare services in order to increase public access by circumventing social and geographic barriers associated with traditional, fixed health care organizations. They provide convenience in delivering health care to communities that may otherwise have restrictions to adequate care due to location, demographic, cost of services, language diversity, limited or no insurance, social stigma or other barriers such as access to transportation.
As reported by U.S. National Library of Medicine and according to the Mobile Health Map Project there are approximately 1,500 MMCs across North America that provide multiple treatment and prevention services to as many as 6.5 million people (not necessarily inclusive with all HRSA grantees). Mobile Medical Clinics provide essential services for those suffering from addictions, substance abuse and other disease specific health concerns.
Additional Sources: